MakAir, an open source ventilator in the making
Published 23 July 2020 by Ewen Chardronnet
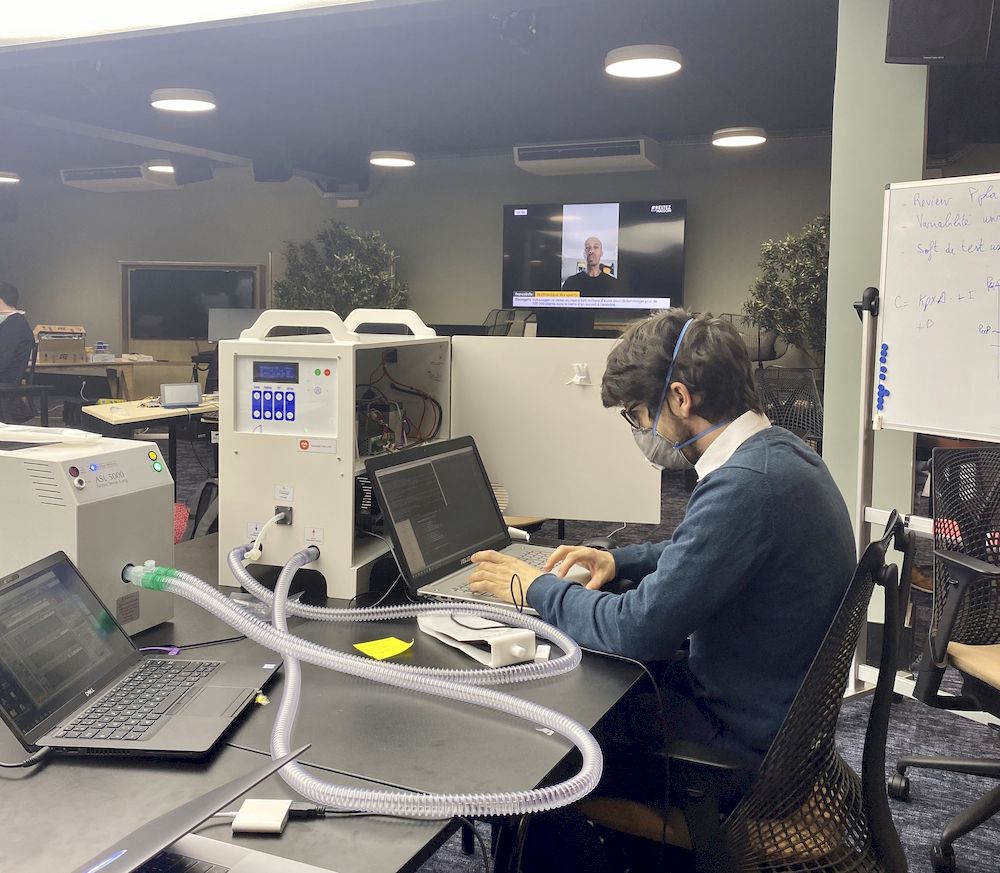
Days after the lockdown began in France, makers and software entrepreneurs in the region of Nantes formed the MakersforLife collective. They soon began to design an open source ventilator: MakAir, a project that has since taken on industrial and international dimensions.
Quentin Adam is the director of Clever Cloud in Nantes, a software company for IT automation. Along with his friends at Crisp, another software company in the region, and Pierre-Antoine Gourraud, who heads the “data clinic” at the CHU (University Hospital), they launched the MakersforLife group to build an open source ventilator called MakAir. This was the beginning of a race for efficiency, which led them to work with the French Alternative Energies and Atomic Energy Commission (CEA) and the Agence de l’innovation de défense (AID). Interview with Quentin Adam, instigator of MakAir.

Makery: How did the MakAir project come about in the context of the lockdown?
Quentin Adam: It was Emmanuel Macron’s “We are at war” speech on March 16 that fundamentally motivated me, made me realize that something was going on. As an entrepreneur, I was already busy with work that was not particularly related to Covid-19. But since my girlfriend works in medicine, I asked her to explain the Coronavirus issue to me. So she explained that the severe acute respiratory syndrome can worsen to the point where people need to be put on ventilators, that the health system will soon be saturated, as there are not enough ventilators currently available, and that given how ventilators are built, it’s very difficult to scale up production in a short period of time, because the components are expensive, because they haven’t been designed to be produced in quantities of 200 a year, etc.
That was when I realized that we needed to produce ventilators. I called Emmanuel Feller, who works with me, Baptiste Jamin and Valérian Saliou at Crisp, and Pierre-Antoine Gourraud at the CHU, to see if they were interested in tackling the design of a ventilator. Our first task was to try to understand what needed to be done, as there are many different types of ventilators. So we sought out anesthetists who could explain what was required for these devices. Most anesthetists don’t actually know how the ventilator is built, what counts for them is its operation and parameters. But a precious few of them were able to provide us with the information we needed to establish a list of specifications and start tinkering.
At the beginning, we didn’t really know what we were doing, but little by little we started to define our aeration system, consolidating each night. As we were working in open source, it wasn’t long before people started to contact us and offer advice. Our only response was: “We’re far from experts, can you help us?” So people got more and more involved, and that’s how we were able to integrate great expertise.

How was the work practically organized in the beginning?
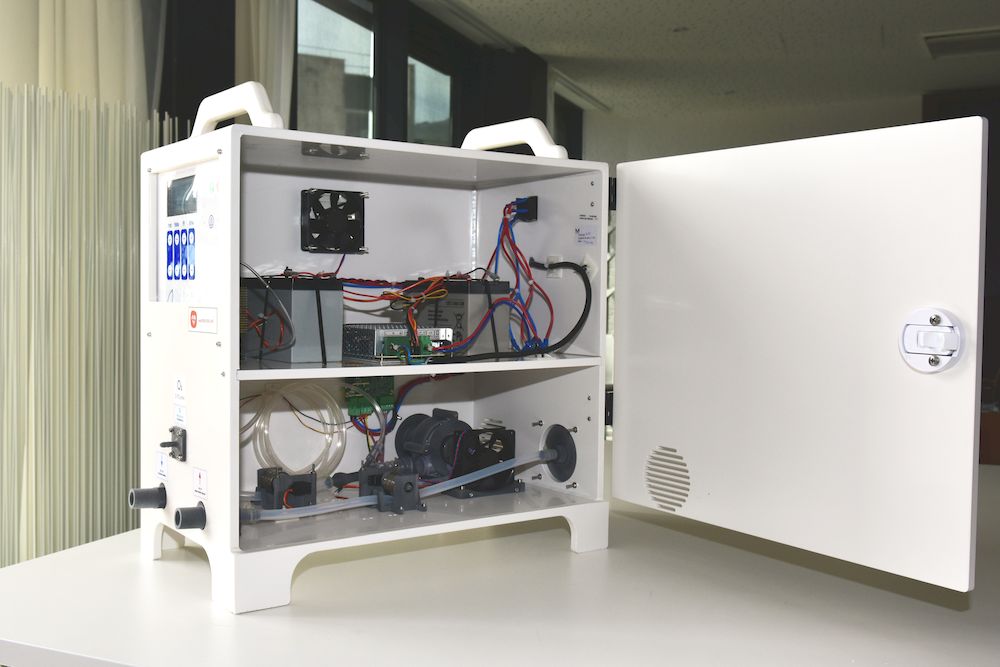
I’m basically a software engineer, I have only a basic knowledge of global engineering, physics, etc. For example, I wasn’t capable of building the electronic circuit board for the MakAir. Neither were any of my initial colleagues. So we relied on experts. We took the approach of a maker, or a software engineer, where instead of starting from a hardware machine running on a bit of software, we started off by designing a software machine, then gradually added what we needed. This is a completely different approach from other ventilators.
So at first, we set out like all the other makers in the world, we used Arduino boards, with defective servomotors, 3D printing, etc. The first versions were terrifying, but we had to advance somehow. On the other side, we researched how we could industrialize and certify our ventilator, because a prototype is useless if you can’t mass produce it and have it certified so that doctors can use it. It was during this quest that I ended up getting a call from Eric Huneker and his associate Marc Julien, directors of the medical company Diabeloop, who offered to help us with regulations. The team was made up of Pierre-Antoine Gourraud in relation with the institutions, Diabeloop on regulations, my initial colleagues on documentation and engineering, and me for general management. Within a week there were a hundred of us, all with well-defined roles.
What obstacles did you encounter once the group of makers became a real “task force” with a specific goal on an industrial scale?
We soon realized that our initial vision of “every hackerspace will be able to produce MakAir” was not feasible, as it’s not the blueprints that are certified, but the industrial production process. So the concept of distributed production, where each one produces three, doesn’t apply, as the machines thenselves will not be standardized. What is possible is to produce one, to work on it and eventually improve it, but afterward production must take place in an industrial space that is identified and certified, with the required ISO standards, etc.
This was a big disappointment for me, as for many makers. So we turned toward something much more industrial. And if 3D printing allowed for rapid prototyping, there isn’t much that’s 3D printed in the current industrial version. Machining is faster, stronger and cheaper. But without 3D printing there would be no MakAir, and we still adopted a maker approach in conceiving the project. Rapid prototyping with 3D printing saved us thousands of hours.

3D printing is just the tip of the iceberg when it comes to makers in action during the Covid crisis…
It was the low-cost accessibility of 3D printing that gave rise to what we now call “makers”. Today a 5-axis CNC machine costs 3,000 euros on AliExpress. Just a few years ago, it was half a million! Now it’s affordable for a maker association. Hackerspaces and makerspaces should really all have one, because it’s a great tool, extremely precise and capable of producing very rigid pieces, as opposed to 3D printing, where the plastics are often porous and emit gas. In our case, you can’t use those plastics for intubation. You could consider SLS, but that’s a whole other price range. The HP Labs machine that we used at the CEA costed half a million euros.
How did MakAir gather so much support so fast, from both makers and industries?
Pierre-Antoine Gourraud, one of the co-founders of the project, is a professor and hospital practitioner at the CHU who co-heads the “data clinic”. He was our link to the CHU and got some of his colleagues involved too. Then after seeing AID’s call for projects, I called Francky Trichet, from Nantes Métropole and the University of Nantes, and convinced him that we had to respond, because many stages of our project, including the clinical trials, would likely be costly. So the teams led by Pierre-Antoine Gourraud and the university worked very conscientiously on submitting our project, and we were finally selected.
Le ministère des Armées soutient le développement d’un respirateur artificiel dédié au traitement du #COVID19
▶️ Projet MakAir : porté par l’@UnivNantes, CHU de Nantes et le collectif Makers For Life
▶️ Financement de l’@Agence_ID : 426 000€#TousMobilisés #FranceUnie pic.twitter.com/50JumzEHjw— Ministère des Armées 🇫🇷 🇪🇺 (@Armees_Gouv) April 27, 2020
The maker community often likes to think of itself as a counter-culture. Not us. For me, it’s a good thing to work with the army. They are efficient people, who know how to do things, and reaching out to them enabled us to realize this project. For example, we were looking for an ASL 5000, the artifical lung that is used to calibrate the machines. A new one costs 55,000 euros, and even if you have the money, it’s hard to find. With Eric and Marc, we set out to get one, we called the French distributor, etc., but we also knew that there was one at the CEA. As Diabeloop is a company associated with the CEA, Eric called Jean Therme (Delegate director for renewable energies), who decided to help us. So the CEA sent us the ASL 5000 and started helping us more and more, up until the point where it was simpler to send our team to the CEA, given the tests that we needed to do.
Scaling up…
One important thing that I want to tell the maker community: we called ourselves “Makers for Life”, but that was a mistake. In fact, from the perspective of the industrial community, makers are more like Sunday hobbyists. Makers need to realize that sometimes they have a divisive attitude about the industry, which offends people who should be allies. Fortunately, our project was perceived as coming from makers but having become industrial, given the makeup of the team. As is often the case in an industrial process, most of us didn’t know each other before, we were basically looking for engineers specialized in each aspect.
What choices did you face once you began working with the army and the CEA?
We were very quickly confronted with the problem of hooking up to the hospital’s oxygen network. We chose not to follow this path, because after discussion with military doctors, we understood that in some cases they would end up intervening in gymnasiums that had been converted into hospitals in rural areas, where there would be no oxygen network. This meant that the project would need to incorporate its own compression bench. That’s why there’s a turbine in our model. In order to optimize the output, we used two ASL 5000s and fed the data into a machine learning optimization loop…
Once we arrived at the CEA, we started to build a pilot line. The supply part was crucial if we wanted to industrialize, for example importing parts from China, Ultem medical plastic, etc. Sandra and Morgane, who had experience working with industrial suppliers, nagged them for information about available quantities, etc. Available supply guided our choices in development. It’s important to understand that engineering was only one aspect of the problem. Knowing the quantity of available stock was crucial, we couldn’t just ask the factory to restart production if we were in short supply.
What happened with the first version, which was released quite early on and attracted a lot of media coverage?
On March 28, we presented a pre-submission to France’s regulatory agency for health products (ANSM). On April 3, we hooked up MakAir Version 1 to a sedated pig, our first pre-clinical trial on an animal after the tests with the ASL 5000. On April 9, we launched the production line and submitted the entire regulatory documentation to ANSM. 60 to 70 machines were produced at the CEA in April. Then we immediately launched the V2, thinking we could improve it, even if the V1 could already save lives. At that time, we believed we would get a quick response from ANSM, but they waited the legal limit of two months to get back to us… So on June 9, we received their response, but only to the V1. Meanwhile we had finished the V2 in May and developed an even better V3 by the end of the month. Right now we’re trying to get the V3 certified directly, and SEB is currently maintaining steady production. The CHU’s Center for Promoting Clinical Trials has now taken over with the V1 and is starting testing the MakAir directly on patients.
All this has crept along a bit slowly for our taste, and without blaming anyone in particular, we still sometimes feel like victims of bureaucracy… In parallel, the will of some countries to initiate the certification process surprised us—some models are already in Madagascar for initial trials. We wonder if building a model with a competitive price point compared with the model of the national manufacturer finally put us at a disadvantage when seeking involvement from certain parties… not easy to see clearly.

How can the MakAir be deployed?
The MakAir can be deployed as a first line of response in rural hospitals. The device can also be customized so that army engineers can understand and repair it, with the option of reconfiguring it remotely depending on the problem. Open source is not just about cost, it’s about innovation. The fact that everyone can participate changes everything. Doctors to whom we sent the MakAir told us that for the past 15 years they had an algorithm to manage air pressure that they couldn’t use on closed machines. But with the MakAir, it’s possible.
In open source, anyone can collaborate. It’s an epistemological breakthrough. Open source medical equipment is fantastic, open data, open code, the possibility for improvement. You can do all your development in open source and then get the industrial process certified. You can create and work within a team, while opening the development up to improvements and advance common knowledge.
After the clinical trials, we will need to have the MakAir re-certified. In the V3 we introduced silent padding and redesigned the model for multi-use, as well as the aeration system, so that parts can be easily changed at low-cost, to avoid the washing process. We’re moving right along.
Presentation of MakAir V3 by Quentin Adam (July 9, 2020):
More about the MakAir ventilator
