Open Insulin, battle of the DIY diabetic
Published 24 April 2018 by Cherise Fong
Well before biohacking junkies were injecting themselves with homemade concoctions, diabetics were hacking their own doses of insulin. At Counter Culture Labs in California, Anthony Di Franco launched the Open Insulin Project to make open source insulin.
Oakland, special report
Type 1 diabetes is an unfortunate disease. Often misdiagnosed and commonly confused with Type 2 diabetes, which has the reputation of being associated with obesity, it is misunderstood by the general public. It mainly affects children, but also adults. It is unpreventable and incurable. There is only one treatment: constant, precisely calculated, expensive doses of insulin. Without these perfectly adjusted doses of the pancreatic hormone, a type 1 diabetic can die within hours.
Access to insulin is a global problem. According to T1International, some 40 million people worldwide live with type 1 diabetes, or 5-10% of all diabetics. The majority of them live in countries where education and health insurance are insufficient. In Sub-Saharan Africa, the life expectancy of a child born with type 1 diabetes is one year.
In the United States, where three big pharmaceutical companies (Eli Lilly, Novo Nordisk, Sanofi) dominate the insulin market, and where their coverage by health insurers is negotiated by three big pharmacy benefit managers (Express Scripts, CVS Health, OptumRx), which benefit from higher prices, the cost of living with type 1 diabetes can be crippling for patients, even with insurance. Some come up with their own ways to save on insulin… often compromising their health to do so. Others die from it.
The cost of insulin by country, charted by T1International:
Anthony Di Franco, computer scientist, type 1 diabetic since 2005 and cofounder of Counter Culture Labs in Oakland, California, launched the Open Insulin Project in 2015, buoyed by a crowdfunding campaign that raised more than $16,000. The project’s objective is to make pure synthetic insulin in a lab, then share the recipe.
Anthony says this initiative emerged from his growing “scepticism” regarding the U.S. pharmaceutical industry in an ultra-capitalist economy. “I’m interested in hacker culture, in any kind of autonomy involving means of producing things that people rely on—closer to the scale of individuals and communities as opposed to corporations, whose interests are very removed from those of the people they’re supposed to serve.”
Unlike the vast majority of medications prescribed in the U.S., there is still no generic form of insulin. While insulin was discovered and developed at the University of Toronto in the early 1920s, the three pharmaceutical giants maintain their oligopoly over insulin to this day—by regularly and slightly modifying their products in order to extend the life of their patents, and probably by paying off newer companies that might otherwise step up to the market.
As a result, over the past decade, the price of insulin has increased fivefold. T1International estimates that Americans spend on average more than $500 each month to treat diabetes. In Brazil or in India, these costs can reach up to 80% of a patient’s monthly income. Hence the hashtag #insulin4all.
"I was testing my blood sugar everyday, but now I have to buy the strips to do it, so I no longer test it everyday. Now, I only do it every month…'' https://t.co/81E15l6PTx #insulin4all pic.twitter.com/vJSvUbS1zU
— T1International (@t1international) April 23, 2018
Currently, the Open Insulin Project is an informal collaboration that counts around a dozen active members at Counter Culture Labs in Oakland, as well as volunteers in a number of labs around the world, such as ReaGent in Ghent (Belgium), BioFoundry in Sydney (Australia), Mboalab in Mvolyé (Cameroon), two groups in Senegal and one in Zimbabwe. Parallel research is also being carried out at the nonprofit organization Fair Access Medicines in California.
“When I launched the project in 2015, as far as I know no one else was working on making insulin,” says Anthony. “But as soon as I publicized what we were doing, many other people decided they wanted to join up. We always hoped that there would be a broader network of people working on these problems and that we could share information and share the fruits of our work. Right now there are more groups in Africa than anywhere else, because they have a very urgent need for basic medical care, including insulin. They also have fewer issues with onerous regulations restricting what they can do. So I expect great things from that part of the collaboration, because their problems are even bigger than the already significant ones we have here.”

Already in the U.S., type 1 diabetics are starting to hack their disease. Because not only are the prices not dropping, the technology is lagging. Most type 1 diabetics (or their parents) must meticulously monitor their glucose levels throughout the day and night, and periodically inject carefully calculated doses of insulin in order to stabilize their metabolism.
Ben West, type 1 diabetic, is one of the pioneers of open source algorithms that connect various monitoring devices and automate the pumping of insulin. His work notably chaperoned the open projects NightScout, a system for remotely monitoring glucose levels in real-time across devices that spurred the #WeAreNotWaiting movement, and OpenAPS (Open Artificial Pancreas System), which evolved into DIYPS (Do-It-Yourself Pancreas System), developed by type 1 diabetic Dana Lewis and her husband Scott Leibrand.
Permanent #Nightscout monitor above my iMac on a used $30 Amazon Kindle Fire. All my important stats at a glance. #Loop #WeAreNotWaiting #T1D #OpenAPS pic.twitter.com/zc0POJILTo
— Alexander Getty (@gettyalex) April 19, 2018
Anthony Di Franco, who studied control theory and closed loop systems at Yale University, explains how they can be applied to diabetes: “Your system is your metabolism, your control input is how much insulin you deliver via the insulin pump and when, then there are blood sugar readings that you can take through continuous monitoring, and you have to put all that together and decide how much insulin to give at what time.”
Closed loop systems can display the patient’s glucose levels in real-time on a mobile connected device, while predicting, calculating and pumping appropriate amounts of insulin according to the patient’s activities. In short, an artificial pancreas. However, the DIYPS still faces two big problems: it’s not officially approved by the U.S. Food and Drug Administration, which limits distribution; it still requires basic programming skills, if not diehard determination, to build. Nonetheless, since 2015 some 600 DIYPS have been built, including by open-minded parents-cum-biohackers.

Among those who are not waiting, three fathers of children with type 1 diabetes—Bryan Mazlish, Jeffrey Brewer and Lane Desborough (cofounder of Nightscout)—came together in San Francisco to launch the start-up Bigfoot Biomedical, an artificial pancreas system created by Mazlish, who believed that going the commercial route was the best way to reach as many people as possible. In late 2017, they raised $37 million to develop their automated insulin delivery system. Since then, clinical trials have begun, and security issues are being taken into account, for an anticipated market launch in 2020.
In parallel, Beta Bionics, a public benefit corporation founded in Massachusetts by Edward Damiano, another father of a type 1 diabetic child, is developing iLet, a commercial “bionic” pancreas system with similarly automated monitoring and delivery functions based on adaptive control algorithms he developed at Boston University with Firas El-Khatib. Interestingly, pharmaceutical giants Eli Lilly and Novo Nordisk have each invested $5 million in Beta Bionics, which also hopes to enter the market within the next few years, pending clinical trials and regulatory approval.
Meanwhile, the nonprofit organization Tidepool has created an open source platform to pool data from diabetes devices to support research and develop software for patients.
All these independent DIY efforts have pushed the industry players to build their own closed loop systems, such as Dexcom Share and Medtronic 670G. While the start-ups believe that artificial pancreas technology is more or less stable, the next challenge remains making it accessible to the wider global community of type 1 diabetics.

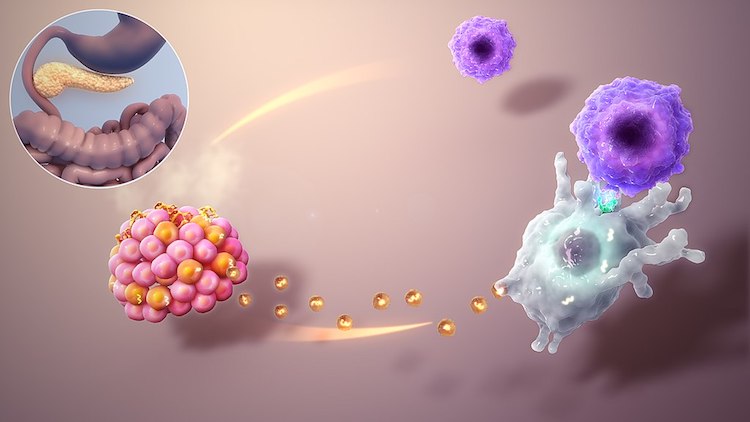
In California, the Open Insulin Project team has so far successfully produced proinsulin from a culture of E. coli bacteria. Now members are working on a yeast culture in an effort to produce mature insulin, which will then need to be purified. “Once we can put production and purification together, that will be the core of how to make insulin,” Anthony explains. “Then we will share that info, we might try to make equipment to automate it, or at least identify how people can get the equipment easily, package it up, share it around, let other people duplicate our work.”
Open Insulin’s other plans include establishing patient-owned and led cooperatives allowing people to make their own medicine or provide them with medicine at low cost. “It might also give us a way to share the costs and efforts associated with doing trials more widely,” Anthony adds, before concluding: “We’re finally at the point where what is behind us is a lot more than what is in front of us. That’s a good feeling.”
Learn more about the situation of Type 1 diabetes in the U.S. in a cartoon by WNYC
Read about our visit to Counter Culture Labs
